- What Is Tube Feeding?
- Why does your Patient need a tube?
- What is Nasogastric Tube (NG Tube) and Percutaneous Gastrostomy Tube (PEG)?
- What is Bolus Feeding and Continuous Feeding?
- What is the equipment that I would need for Homecare Adult Patient?
- What do I feed my patient?
- Complications in Tube Feeding and How I should Address them?
- When should I reach out for Professional Help?
- Getting support for Feeding Instructions for Ng Tube right at home with The Food Balance Clinics.
- Conclusion
What Is Tube Feeding?
Tube Feeding or Enteral Nutrition is a medical intervention in which a tube is used to deliver liquid nutrition through your nose, or stomach into your digestive system. It is used when a patient is unable to meet his normal nutritional needs through oral intake.
Why does your Patient need a tube?
If the patient is unable to take oral nutrition and is unable to meet his caloric requirements, there is a risk of
malnutrition and other serious health issues. Therefore, your doctor may decide to put in a tube for a temporary
period as short as a few days or weeks, or permanently for as long as your loved one may need.
There are several medical conditions such as stroke, cancer, traumatic brain injury, and gastrointestinal orders
that may need the support of a tube feeding to ensure dietary requirements are met.
What is Nasogastric Tube (NG Tube) and Percutaneous Gastrostomy Tube (PEG)?
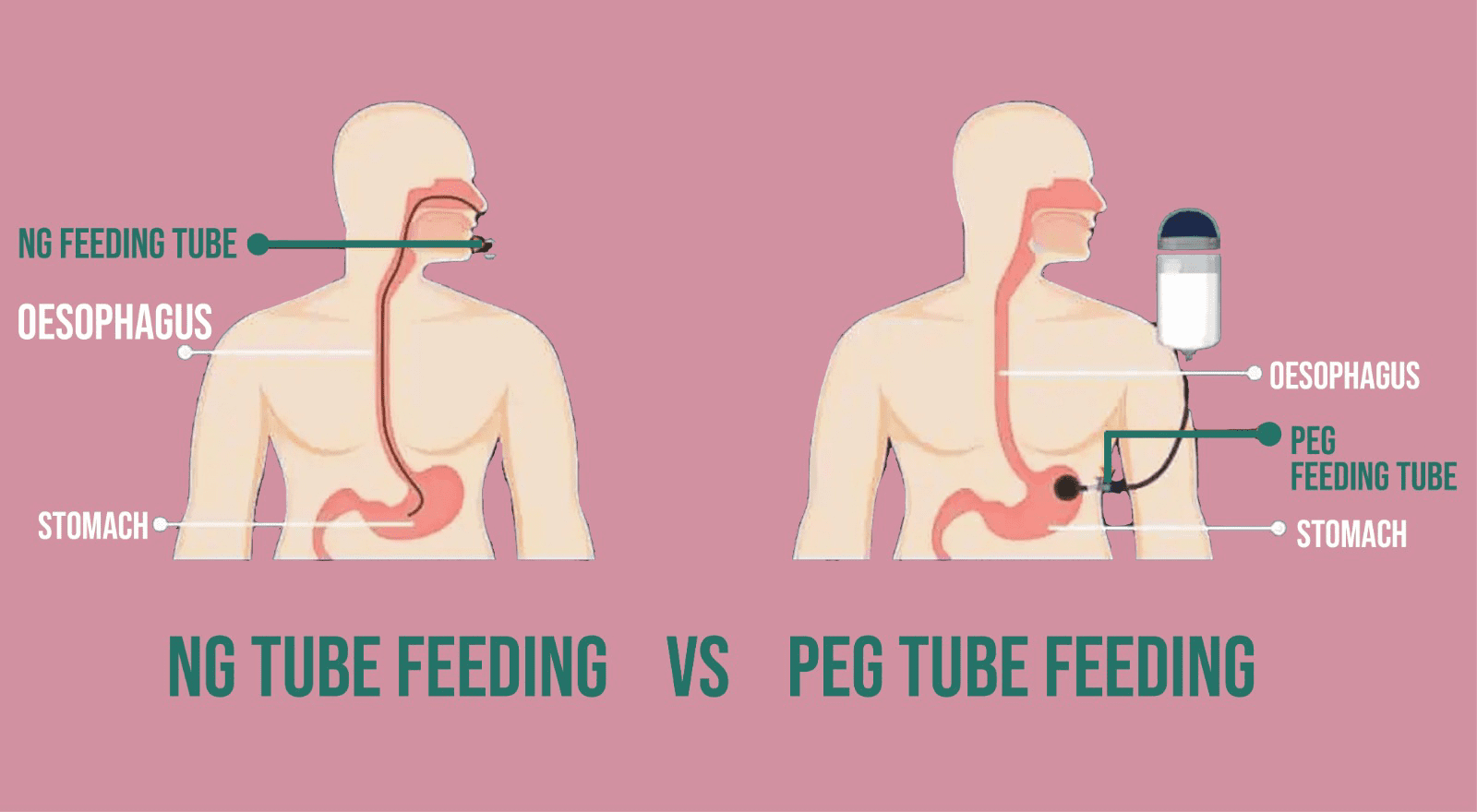
Naso gastric Tube Feeding (Ng) is the most common feeding route used in hospitals in Pakistan. This tube is
inserted through the nose into the patient’s food pipe (esophagus) and then into the stomach. It is used when an
individual requires short-term nutritional support.
Gastric tube feeding also called Percutaneous Endoscopic Gastrostomy tube is a type of tube that is surgically
placed in the hospital directly into the stomach. It is used when the patient requires support of enteral nutrition
for an extended period of time.
What is Bolus Feeding and Continuous Feeding?
The Bolus Feeding method is used usually when the patient is being released from the hospital. A large volume of
formula feed is given several times a day. It could be after every 3 to 4 hours.
Continuous feeding is most commonly used during hospitalization, and an electronic pump is required which provides
the formula slowly in small amounts over hours. It helps to reach caloric goals and is recommended for patients
experiencing nausea and vomiting.
What are the Equipments that I would need for Homecare Adult Patient?
While you are preparing for home feeding at home it requires specific equipment to ensure the safe administration of the liquid formula through the tube. The exact equipment needed can vary based on the route of feeding prescribed and the individual needs, but here is a general list of items:
Tube Feeding Formula:
A specialized liquid balance nutrition formula is needed which is designed for tube
feeding.
Many different types of formula exist but the one for your family is decided by your registered dietitian. The
selection usually depends on the patient’s medical conditions, dietary restrictions, and nutritional needs and
requirements.
Tube Feeding Pump:
A pump is used to control the total amount of feed and the rate of the formula feed to ensure timely flow. This method is usually administered when bolus feeding is not well tolerated.
Feeding Tube:
The feeding tube is inserted by the nursing staff at the hospital or a homecare staff at the bedside at home. It could be made of PVC, Silicone, or polyurethane and comes in different sizes.
Cleaning Supplies:
Items such as gauze for cleaning, mild soap, and pair of gloves are needed to clean around the tube feeding site.
Measuring Cup or Syringe:
You would need a 60 ml syringe to measure and administer prepared feeding, and additional fluids.
What do I feed my patient?
Here you would need an instructed calorie counted and protein counted plan with the amount and schedule. Be sure to
follow the given instructions. The plan is usually made by our expert registered dietitian.
Administering feeding through an NG or Peg tube seems overwhelming at first but the nursing staff in all the
hospitals train family members. Be sure to get your training on how to feed at home. Also, Feeding should always be
administered at room temperature.
Complications in Tube Feeding and How I should Address them?
As you transition through the journey of tube feeding complications may arise. You may have to be mindful and ensure safe tube feeding practices are being followed. Hence, it is very important to know what sort of problems to look out for and how to address each of them either by yourself or through professional help.
Tube Displacement:
While administering feed if you find difficulty flushing the feed it could be a sign that the tube has been displaced. In addition to this, the patient may experience or show signs of abdominal discomfort which is also an indicator of the problem with the tube position. In the case, of a nasogastric tube increased persistent coughing or increased breathing may indicate tube displacement.
Tube Leakage:
If you see liquid seeping out from the site of the gastric tube may indicate signs of tube displacement. In this case, you need to seek medical professional help.
Tube blockage:
If you experience a backflow in the contents or slow passage of content of food, kindly seek medical help. This usually indicates that the tube is blocked, preventing the food from passing into the stomach or intestines.
Diarrhea and Vomiting:
The first important step is to identify the cause of Diarrhea and vomiting. This is a very common happening and it could be due to formula concentration, formula composition, rate of administration, inadequate water intake, infection, medication side effects, underlying gastric issues such as intolerance to specific nutrients, and bacterial overgrowth. It is important here to reach out to your registered dietitian and they will make dietary-related changes to your enteral nutrition plan. If diarrhea persists kindly reach out to your attending physician immediately.
Infection:
Two types of infection can be observed while the patient is being tube fed. Local
infections are observed around the site of the tube feeding. It could be a skin infection due to bacteria
penetrating the area or it could be granulation tissue which occurs due to prolonged irritation or friction from the
tube that can cause the site to become infected. In both types of local infection, proper hygiene, including regular
cleaning of the site of the tube can help prevent skin infections, and observance of local sites may prevent these
damages to the skin from happening.
In the case of Systemic infection Aspiration Pneumonia is the most commonly observed sign in which gastric contents
may enter the lungs which can cause Pneumonia. In this case, always ensure that the head of the bed is elevated
during and after feeding.
Signs and symptoms of infection include fever, chills, and increased heart rate.
These should be addressed immediately.
When should I reach out for Professional Help?
These include but are not limited to:- Initial training on how to tube feed.
- Regular follow-ups with a registered dietitian and your physician.
- Nutritional assessment and your tube feeding plan
- Tube displacement
- If the patient is persistently vomiting
- If the patient is coughing up food
- Changes in Medical Conditions such as high-grade fever
- Unintentional weight loss
- Persistent symptoms of Malnutrition
- Bedsores
- Changes in medication if required
Getting support for Feeding Instructions for Ng Tube right at home with The Food Balance Clinics.
Our Dietitian has years of experience with prescribing the right nutrition and has catered to 1000 of patients with their plans suited to their needs. We provided calorie-counted nutrition care plans such as what to feed, how to feed, and when to feed. Contact us when you need a dietitian consultation. We only provide services through virtual care.
Conclusion
In conclusion, effectively managing the complexities of tube feeding and feeding tube maintenance, including Nasogastric (NG) tubes, within the context of home care necessitates a combination of knowledge, preparation, and continuous vigilance. You and your loved ones can establish a secure and supportive setting by acquiring knowledge regarding the various types of feeding tubes, techniques, and essential equipment.
Various complications can arise throughout the process of tube feeding, including infections and displacement; therefore, it is essential to promptly identify and attend to them. Consistent communication with healthcare practitioners, such as dietitians and physicians, is vital to developing a comprehensive care strategy.

